前言
隆乳手術的切口可分為腋下(Trans-axillary),乳暈旁(Peri-areolar),胸下緣(Inframmary fold)與肚臍切口(Umbilical),每個切口各有其優劣之處,此篇文章是吳至偉醫師醫師多年心得,旨在探討胸下緣隆乳之優劣處。
為何胸下緣隆乳?
簡單來說,胸下緣隆乳有下列好處:
- 手術時間短
- 出血少
- 疼痛度低
- 恢復快
- 術後照顧容易
胸下緣隆乳(IMF incision breast augmentation)是一個歷史悠久的整形手術,也是美國與歐洲整形外科醫師最常使用來施行隆乳手術的方式,但是在亞洲地區,則因許多醫師對於疤痕的掌控觀念不佳,造成不少難看的疤痕,因此常被誤解為不好的手術方式,但事實上,如果一位整形外科醫師對於傷口縫合,張力控制與疤痕照顧的觀念是錯誤的,那不論是胸下緣切口,乳暈旁切口,或是腋下切口,最後的疤痕結果都極少令人滿意。因此不少醫師爭論疤痕應該在胸下緣或是腋下,其實意義不大,應該爭論的重點是醫師的技術,一位好醫師,不論是胸下緣切口或是腋下切口,在多數的案例中都可以得到令人滿意的疤痕結果(或即使疤痕不夠漂亮,但因技術層次到位,經過修疤手術後,亦可以達到令人滿意的結果)。
手術時間
隆乳手術包含幾個步驟:皮膚切口,胸部空間剝離,果凍矽膠置放,位置調整,傷口縫合。胸部空間剝離要精準且流血要少,單側至少要花20-60分鐘,雙側則至少40-120分鐘,以胸下緣隆乳而言,如果醫師技術純熟,應可控制在90分鐘完成上述步驟。而較短的手術時間,意謂著較快的恢復期與較少的併發症。
術後照顧容易
以腋下切口隆乳而言,術後以胸帶綁上胸部加上穿著手術胸罩是必需的(通常需至少一個月);而胸下緣切口隆乳,則通常不需胸帶,亦不需手術胸罩,減少術後照顧的不便,讓隆乳的恢復變得簡單與快速許多。
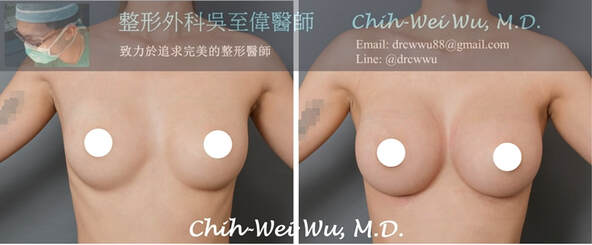
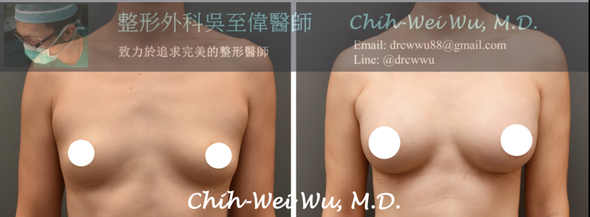
胸下緣隆乳疤痕狀況
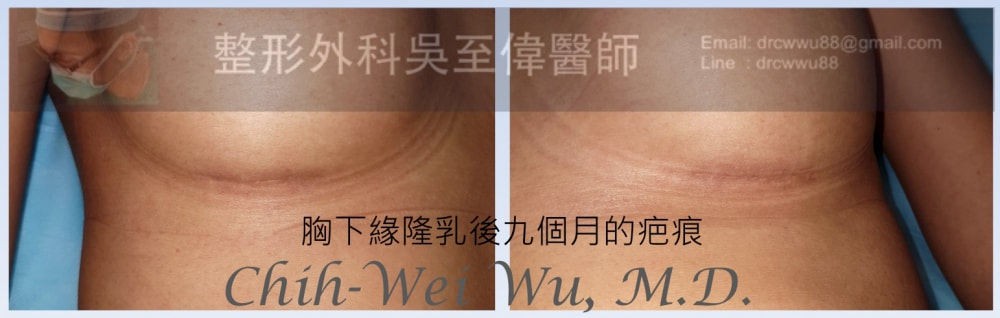
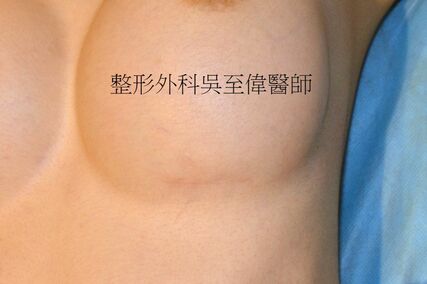
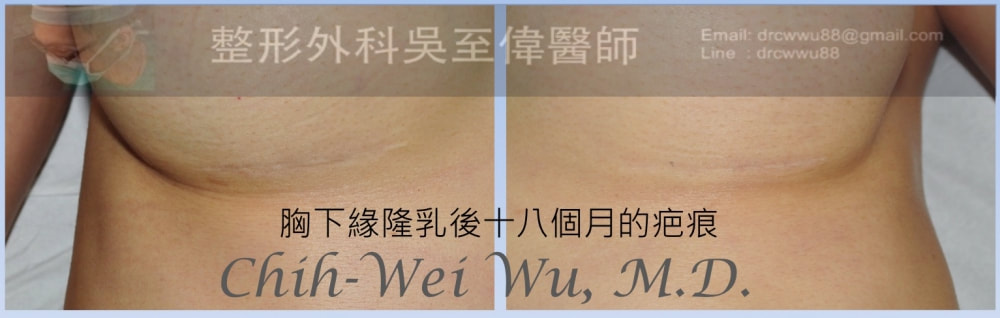
胸下緣隆乳疤痕的癒合狀況與其他部位相同,一開始的疤痕會是紅色的,約3個月會進入反黑期,反黑期的長短視個人膚質而有所不同,經過良好照顧與適當的疤痕療程,在6-12個月之間會慢慢變淡,約在術後一年半會達到最淡化的效果。疤痕恢復過程如下圖所示,但效果因人而異:
胸下緣隆乳的恢復期
一般而言,胸下緣隆乳後,比較明顯的疼痛約在前三天(亦有人開刀完就不太痛的),比較腋下切口,恢復期是短上許多,對於不少時間有限的上班族女性朋友,是非常適合的選擇。
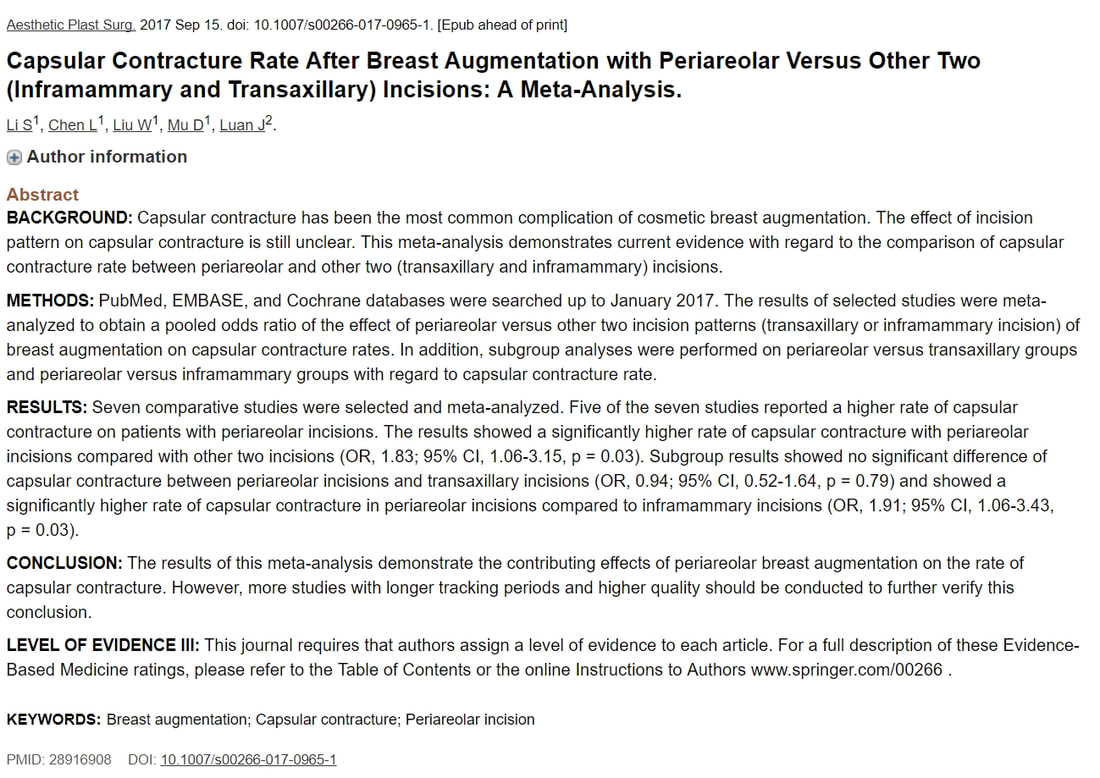
最新論文證實胸下緣隆乳有最低的莢膜攣縮比例
2017年九月發表於Aesthetic Plastic Surgery的一篇大規模統計文章(Meta-analysis),統計經由不同切口隆乳時的莢膜攣縮比例,發現隆乳後莢膜攣縮比例最高的是乳暈旁切口,而最低的則是胸下緣切口。詳見:【不同隆乳切口的莢膜攣縮比例】
BACKGROUND:
Capsular contracture has been the most common complication of cosmetic breast augmentation. The effect of incision pattern on capsular contracture is still unclear. This meta-analysis demonstrates current evidence with regard to the comparison of capsular contracture rate between periareolar and other two (transaxillary and inframammary) incisions.
METHODS:
PubMed, EMBASE, and Cochrane databases were searched up to January 2017. The results of selected studies were meta-analyzed to obtain a pooled odds ratio of the effect of periareolar versus other two incision patterns (transaxillary or inframammary incision) of breast augmentation on capsular contracture rates. In addition, subgroup analyses were performed on periareolar versus transaxillary groups and periareolar versus inframammary groups with regard to capsular contracture rate.
RESULTS:
Seven comparative studies were selected and meta-analyzed. Five of the seven studies reported a higher rate of capsular contracture on patients with periareolar incisions. The results showed a significantly higher rate of capsular contracture with periareolar incisions compared with other two incisions (OR, 1.83; 95% CI, 1.06-3.15, p = 0.03). Subgroup results showed no significant difference of capsular contracture between periareolar incisions and transaxillary incisions (OR, 0.94; 95% CI, 0.52-1.64, p = 0.79) and showed a significantly higher rate of capsular contracture in periareolar incisions compared to inframammary incisions (OR, 1.91; 95% CI, 1.06-3.43, p = 0.03).
CONCLUSION:
The results of this meta-analysis demonstrate the contributing effects of periareolar breastaugmentation on the rate of capsular contracture. However, more studies with longer tracking periods and higher quality should be conducted to further verify this conclusion.
Capsular contracture has been the most common complication of cosmetic breast augmentation. The effect of incision pattern on capsular contracture is still unclear. This meta-analysis demonstrates current evidence with regard to the comparison of capsular contracture rate between periareolar and other two (transaxillary and inframammary) incisions.
METHODS:
PubMed, EMBASE, and Cochrane databases were searched up to January 2017. The results of selected studies were meta-analyzed to obtain a pooled odds ratio of the effect of periareolar versus other two incision patterns (transaxillary or inframammary incision) of breast augmentation on capsular contracture rates. In addition, subgroup analyses were performed on periareolar versus transaxillary groups and periareolar versus inframammary groups with regard to capsular contracture rate.
RESULTS:
Seven comparative studies were selected and meta-analyzed. Five of the seven studies reported a higher rate of capsular contracture on patients with periareolar incisions. The results showed a significantly higher rate of capsular contracture with periareolar incisions compared with other two incisions (OR, 1.83; 95% CI, 1.06-3.15, p = 0.03). Subgroup results showed no significant difference of capsular contracture between periareolar incisions and transaxillary incisions (OR, 0.94; 95% CI, 0.52-1.64, p = 0.79) and showed a significantly higher rate of capsular contracture in periareolar incisions compared to inframammary incisions (OR, 1.91; 95% CI, 1.06-3.43, p = 0.03).
CONCLUSION:
The results of this meta-analysis demonstrate the contributing effects of periareolar breastaugmentation on the rate of capsular contracture. However, more studies with longer tracking periods and higher quality should be conducted to further verify this conclusion.
最新論文:胸下緣隆乳切口與腋下隆乳切口的疤痕狀況是相同的
來自北京協和醫院的研究,在分析163個患者的疤痕後,發現在12個月的長期追蹤,腋下與胸下緣疤痕的狀況可得到接近的美觀結果,證實胸下緣切口隆乳在華人女性也是一個好的選擇。
Aesthetic Plast Surg. 2019 Apr;43(2):328-335. doi: 10.1007/s00266-018-1299-3. Epub 2019 Jan 3.
The Comparison of Scars in Breast Implantation Surgery with Inframammary Fold Incision Versus Axillary Incision: A Prospective Cohort Study in Chinese Patients.
Sun J1, Mu D1, Liu C1, Xin M1, Fu S1, Chen L1, Liu W1, Luan J2.
Abstract
BACKGROUND:
A prospective cohort study was developed to compare the surgical scars in the axilla and the inframammary fold at short-, medium- and long-term time periods after surgery.
METHODS:
Patients who underwent primary breast augmentation with implants in our department were divided into two groups based on the incision location they chose and were followed up for scar assessment at 1 month, 6 months and 12 months post-surgery from June 2012 to March 2016. Each scar was evaluated by the Vancouver Scar Scale (VSS) and patient satisfaction score. The data were analyzed with Wilcoxon rank-sum tests, Cochran-Armitage trend tests and Fisher's exact probability tests based on the data type.
RESULTS:
One hundred and sixty-three patients were completely investigated three times. Ninety-four patients underwent breast augmentation surgeries with implants through axillary approaches and 69 patients through IMF approaches. At 1 month after surgery, the median total VSS score was 6 in the axillary incision group and 4 in the IMF group, with statistically significant differences (P < 0.05). Larger proportions of high scores in terms of vascularity and height were found in the axillary incision group (P < 0.05). At 6 months after surgery, the median total VSS score was 4 in the axillary incision group and 3 in the IMF group, with statistical significance (P < 0.05). The axillary group still had a larger proportion of high scores in terms of vascularity and height than that of the IMF group (P < 0.05). At 12 months after surgery, the median total VSS score was 2 in both groups. The median patient satisfaction score was 9 in both groups. No significant differences were noted in the total VSS and patient satisfaction scores between the two groups. However, the axillary group had a larger proportion of high scores in terms of vascularity and low scores in terms of pliability.
CONCLUSIONS:
The total VSS score for the axillary incision group was significantly higher than that for the IMF incision group one and 6 months after surgery, mainly on the subscales of vascularity and height. At 12 months after surgery, the total VSS scores were not different between the two groups, and patients with both kinds of incisions were highly satisfied with scar appearance. The research confirmed that the scars at two locations can achieve comparable appearance in the long term after surgery.
The Comparison of Scars in Breast Implantation Surgery with Inframammary Fold Incision Versus Axillary Incision: A Prospective Cohort Study in Chinese Patients.
Sun J1, Mu D1, Liu C1, Xin M1, Fu S1, Chen L1, Liu W1, Luan J2.
Abstract
BACKGROUND:
A prospective cohort study was developed to compare the surgical scars in the axilla and the inframammary fold at short-, medium- and long-term time periods after surgery.
METHODS:
Patients who underwent primary breast augmentation with implants in our department were divided into two groups based on the incision location they chose and were followed up for scar assessment at 1 month, 6 months and 12 months post-surgery from June 2012 to March 2016. Each scar was evaluated by the Vancouver Scar Scale (VSS) and patient satisfaction score. The data were analyzed with Wilcoxon rank-sum tests, Cochran-Armitage trend tests and Fisher's exact probability tests based on the data type.
RESULTS:
One hundred and sixty-three patients were completely investigated three times. Ninety-four patients underwent breast augmentation surgeries with implants through axillary approaches and 69 patients through IMF approaches. At 1 month after surgery, the median total VSS score was 6 in the axillary incision group and 4 in the IMF group, with statistically significant differences (P < 0.05). Larger proportions of high scores in terms of vascularity and height were found in the axillary incision group (P < 0.05). At 6 months after surgery, the median total VSS score was 4 in the axillary incision group and 3 in the IMF group, with statistical significance (P < 0.05). The axillary group still had a larger proportion of high scores in terms of vascularity and height than that of the IMF group (P < 0.05). At 12 months after surgery, the median total VSS score was 2 in both groups. The median patient satisfaction score was 9 in both groups. No significant differences were noted in the total VSS and patient satisfaction scores between the two groups. However, the axillary group had a larger proportion of high scores in terms of vascularity and low scores in terms of pliability.
CONCLUSIONS:
The total VSS score for the axillary incision group was significantly higher than that for the IMF incision group one and 6 months after surgery, mainly on the subscales of vascularity and height. At 12 months after surgery, the total VSS scores were not different between the two groups, and patients with both kinds of incisions were highly satisfied with scar appearance. The research confirmed that the scars at two locations can achieve comparable appearance in the long term after surgery.
此篇論文發表在aesthetic plastic surgery 2019年4月號,比較了94個腋下切口隆乳與69個胸下緣切口隆乳的案例疤痕狀況〔使用Vancouver Scar Scale,為一客觀之疤痕評估方式〕,在術後六個月追蹤時,胸下緣隆乳的疤痕明顯比腋下隆乳的疤痕好,在術後12個月追蹤時,兩組則沒有明顯差異〔At 12 months after surgery, the total VSS scaores were not different between the two groups〕。